For patients
Pediatric interventional radiology
Pediatric interventional radiologists (PIRs) are specially trained to deliver minimally invasive care to infants, children and teenagers. The treatments they deliver carry less risk, less pain and less recovery time than traditional surgery.

What is pediatric interventional radiology?
Pediatric interventional radiologists (PIRs) are specially trained to deliver minimally invasive care to infants, children and teenagers. The treatments they deliver carry less risk, less pain and less recovery time than traditional surgery. PIRs generally have additional training in interventional radiology therapies for children. Like most interventional radiology treatments, care for younger patients is also delivered via catheters (long, skinny, soft, blunt-ended tubes) or other devices through a tiny nick in the skin and use different types of radiology imaging guidance, including X-rays, CT scanning and ultrasound, to deliver precise treatment. Many treatments are performed on an outpatient basis or with a short hospital stay.
What are the advantages of pediatric interventional radiology treatments?
Interventional radiology treatments generally offer less risk, less recovery time and less pain in the recovery process compared to open surgery. Therefore, children are generally out of bed and back to school and play sooner than other options.
What treatments do pediatric IRs offer?
Pediatric interventional radiologists treat many medical conditions that affect infants, children and teenagers. A referral may be needed from a pediatrician, family practitioner or specialist.

Common conditions and treatments include:
Vascular anomalies
IRs are experts in the treatment of abnormal blood vessel development. In the womb, sometimes arteries and veins connect to one another in an abnormal fashion, resulting in abnormal blood flow, associated pain and sometimes other symptoms. These malformations can be physically debilitating or psychologically damaging to a child’s development.
Using their expertise in performing embolization, sclerotherapy and/or laser treatments, IRs help address the associated symptoms of these malformations and, in some cases, help children feel better about their appearance. Sclerotherapy is a medical word for any treatment designed to decrease the size and activity in a vascular malformation by causing the malformation to undergo a scarring process that decreases its size over time.
An example is treatment applied arteriovenous malformations (AVMs) and telangiectasias caused by conditions such as hereditary hemorrhagic telangiectasia (HHT), an inherited vascular disorder.
Deep vein thrombosis
Blood clots in the pelvis and legs can be fatal. Interventional radiologists use medications and devices to help break up blood clots and open blood vessels that have been closed by clots, which can help reduce long-term damage from them.
Feeding difficulties
An interventional radiologist can safely insert a small tube (catheter) directly into the stomach or small intestine of children under intravenous sedation or general anesthesia. This tube helps children who are unable to take sufficient food by mouth. In short-term situations, the IR may insert the tubes via the nose or mouth.
Biliary drainage
A biliary-enteric stricture is a narrowing or blockage of the passages in the liver that drains digestive chemicals (bile) from the liver into the small intestine, which can sometimes occur in children who have undergone liver transplantation. If that happens, a pediatric IR uses a special catheter with a balloon attached to the end of it to open the bile passages, thus unblocking the backed-up fluid in the liver passage.
To do so, an interventional radiologist passes a needle through the skin and into the liver, using ultrasound and X-ray for guidance. Once there, the doctor uses a liquid agent that shows up on X-ray, called contrast, to watch the flow of the digestive chemicals, or bile, through the liver passage and identify the narrowed part of the passage. The congestion in the liver is relieved by opening the blocked area with the specialized balloon catheter or other specialized tools.
Central venous access
A thin, plastic tube (catheter) is safely inserted into a vein so that fluid, nutrition, medication or chemotherapy can be injected into the bloodstream. Central venous access catheters reduce the need for repeated needle sticks for blood removal and drug injections. The types of catheters that may be placed include peripheral catheters in the arms (peripherally inserted central catheters, or “PICC lines”) or catheters in the neck or leg called “central lines.” A port—a small, specialized catheter device used to make repeated venous injections easier and less painful—is usually placed in the chest area, though in younger children it may be placed in the abdomen. The insertion will require at least some type of sedation or anesthesia in most children.
Biopsy
In a biopsy, an IR takes small samples of tumors in organs (e.g., liver or kidney) or other non-tumor lesions to determine whether the tumor or lesion will require further treatment or can be left alone (benign). The biopsy itself is performed with only a needle via a small nick in the skin no bigger than a small freckle. Anesthesia is used to make the patient comfortable. An IR will use ultrasound, fluoroscopy and/or CT to help guide the needle through your child’s skin and into the tumor to take the sample.
Diagnostic angiography
A small plastic tube (catheter) is placed into an artery, injecting a liquid material that shows up on X-ray, called contrast, while X-rays are taken of the area. This kind of imaging helps diagnose vascular problems anywhere in the body, blood vessel malformations, high blood pressure, liver disease or other conditions.
Other common interventional radiology treatments performed in infants and children include diagnosis and drainage of infections, unclogging blocked blood vessels, and treating blockage of blood flow to the kidneys and other kidney problems.
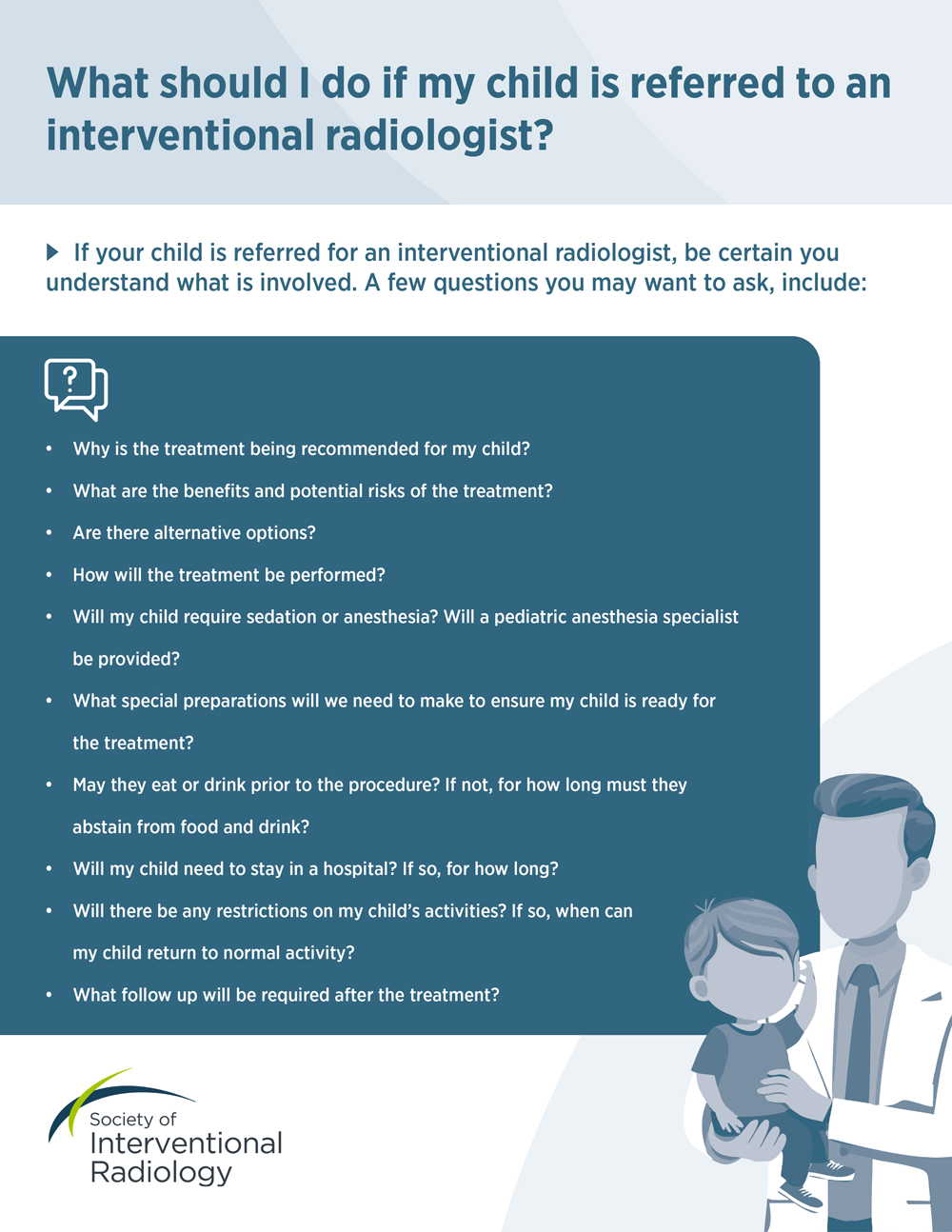
If your child is referred for an interventional treatment, be certain you understand what is involved. Download, print and save this list of questions you may want to ask at your consultation.
What should you expect after treatment?
Once the treatment is completed, the doctor removes the catheter and any other small devices. Then they apply pressure to the tiny incision to allow the small needle poke to stop bleeding. Usually, your child will be able to go home the same day, but there is a small chance he or she will require a short stay at the hospital. After the treatment, your child may be prescribed medication to assist with any pain or healing. During a period of regular follow-up appointments, which may include ultrasound or other imaging tests, the doctor will monitor your child’s progress after the therapy.
RecoveryDue to the minimally invasive nature of the treatments performed by an IR, the recovery time is often just a few days.
Follow-upThe interventional radiologist is part of the clinical care team and will work closely with the other physicians and members of the healthcare team to ensure that your child receives the best possible care. This includes follow-up during hospital stays and after your child is discharged. During the follow-up appointment, the PIR will evaluate your child’s progress and address any remaining issues or symptoms that he or she may have.

Use SIR's Doctor Finder to search for interventional radiologists in the United States and abroad.
Reviewed by Theodore B. Gupton, MD, November 2024