For patients
Superficial venous disease
Superficial veins are those close to the surface of the body. Superficial venous disease is a common clinical problem also known as “chronic venous insufficiency” or “venous reflux.”
Signs and symptoms
What is superficial venous disease?
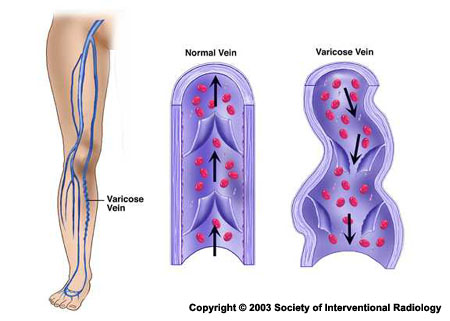
Superficial veins are those close to the surface of the body. Superficial venous disease is a common clinical problem also known as “chronic venous insufficiency” or “venous reflux.” In those with venous insufficiency, the walls of the veins have become weakened and/or the valves in the veins are leaky, both of which cause blood to “reflux,” or move in the wrong direction towards the ankles and feet, instead of towards the heart. This leads to pooling of blood in the veins of the legs causing symptoms of pain, heaviness and swelling.
What are the types of superficial venous disease or “chronic venous insufficiency”?
- Venous reflux occurs when vein walls are weakened and the valves that normally force blood in your veins up towards your heart no longer function, causing blood to pool up in the legs and the veins to become distended. Superficial venous reflux can be a significant contributor to wounds caused by chronic venous insufficiency. Superficial venous reflux has been associated with an increased risk of deep vein thrombosis.
- Varicose veins are dilated and elongated veins that often are visible just under the surface of the skin. This is a common condition is caused by venous reflux. Varicose veins can lead to chronic pain, heaviness, aching throbbing and swelling. In severe cases it can result in nonhealing skin wounds in the lower calf and by the ankle.
- Superficial venous thrombosis is the combination of blood clots (thrombosis) and inflammation in a superficial vein.
While superficial venous disease may sound minor due to its name, it can lead to more serious complications, such as deep venous diseases, and should be treated a doctor, such as an interventional radiologist. An interventional radiologist can diagnose these conditions by history, physical examination and ultrasound, an imaging procedure where a probe is placed on the skin to take images and real-time videos of the vein using sound waves.
Minimally invasive options
How do IRs treat superficial venous disease?
Initial treatments are conservative and include lifestyle changes as well as medication.
- Leg elevation and getting regular exercise
- Usage of compression stockings
- Decreased time spent standing and sitting
- Walking more frequently
- Medications designed to improve “strength” of veins and help them return blood to the heart
If these lifestyle changes don’t fix the problem, your interventional radiologist may recommend a minimally invasive treatment. Those treatments typically close off the diseased vein, allowing blood to return through healthy veins.
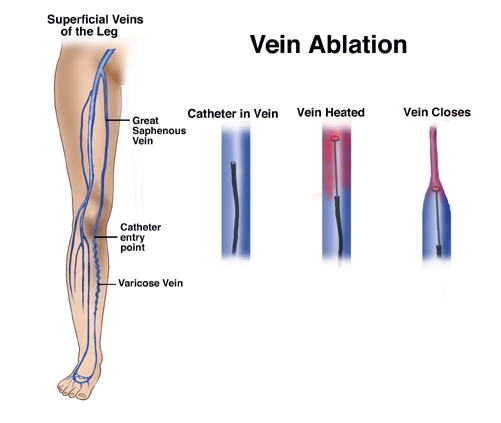
Endovenous laser ablation treatment (EVLT)
The diseased vein is closed by heat from a thin laser that is inserted through a small needle.
Radiofrequency ablation
The diseased vein is closed by heat from radio waves emitted by a thin wire inserted through a small needle.
Microphlebectomy
The diseased vein is removed through tiny skin incisions.
Sclerotherapy
Small diseased veins are closed by injecting, through tiny needles, a solution that causes the walls of the blood vessel to stick together.
How are the treatments performed?In an outpatient office, the interventional radiologist often performs this with local numbing medicine only. They may offer you “conscious sedation” to help calm you during the procedure if necessary.
The interventional radiologist places a small needle into the diseased vein under guidance of ultrasound.
Patients go home on the same day with a small bandage placed over the needle puncture. They can immediately return to most normal day-to-day activities such as walking, sitting and standing, avoiding heavy lifting or strenuous exercise 1–2 weeks. If a microphlebectomy is done, a dressing may be placed over the area and removed in a few days according to your doctor’s instructions.
Follow up and recovery
Life after treatment
What is the treatment’s recovery like?
Due to the minimally invasive nature of the treatments performed by interventional radiologists, the recovery time is often brief but varies with the individual patient’s needs. Patients are often able to walk immediately after varicose vein treatment and encouraged to do so to prevent blood clots. Patients can go home immediately and resume their usual activities that day with the exception of heavy lifting or strenuous exercise, which may be resumed after about a week.
Consult your doctor to see if specific activities should be avoided during this time, such as long car rides or plane flights. You should also avoid hot tubs and saunas for 2 weeks as they may open treated veins.
You may experience mild pain and soreness after treatment as the veins respond to treatment. This is normal and you can take Tylenol or ibuprofen to manage the pain. You may also feel inflammation and bruising on the skin surface near the point of treatment, and a tightening of the ablated veins or the development of lumps at the site of treatment. These usually resolve quickly, within 1–2 months.
Depending on your treatment, you may need to wear compression stockings during the first few weeks after the procedure while the veins recover. At 3 months post-procedure, many patients have complete resolution of symptoms with disappearance of varicose veins.
What is the follow-up care like?
Your interventional radiologist is part of your clinical care team and will work closely with you to ensure that you receive the best possible care. During your follow-up appointment, your interventional radiologist will evaluate your progress and address any remaining issues or symptoms that you may have.
What are the risks associated with these treatment options?
While complications are rare, all procedures carry some risk. The risks associated with superficial vein treatments include:
- Severe bruising and pain, which generally resolves after a few weeks. If you take blood thinners such as aspirin, Plavix, or coumadin, and this occurs, contact your doctor immediately.
- Prolonged redness and tenderness around the puncture sites or over the treated vein segment. If you see pus from the puncture sites, call your physician immediately or go to the emergency department as this may be a sign of a more serious infection.
- Deep vein thrombosis, which are clots extending into the important deep veins, can occur. This potentially serious complication is uncommon if the protocol of compression and regular daily walking are followed. If this is demonstrated on the postoperative scan, you may require treatment with daily heparin injections until further scans show the clot is resolving.
- There is a risk of stroke during the treatment, but this is exceedingly rare.
- Recurrence. Treated veins can reopen or new veins can develop.
Reviewed by Venous Clinical Specialty Council. September 2024.